
All You Need To Know About the Link Between PPS and Disturbed Sleep
October 21, 2022
How Diabetes During Pregnancy Threatens Foetal Health
November 23, 2022Clinical trials that have investigated if postprandial-blood-glucose—lowering treatment does indeed reduce the risk of cardiovascular disease (CVD) in those with diabetes have so far fielded mix results. That said, this surely does not rule out the possibility of hyperglycaemia playing a significant role in promoting CVD or elevating its risk.
In reality, lowering postprandial blood sugar seems to help in promoting certain beneficial long-term effects, and CGM (continuous glucose monitoring) devices have indicated that postprandial sugar (PPS) spikes of hyperglycaemia occur quite frequently, making it an important determinant of the risk of developing CVD.
It has been proposed that these short and intermittent hyperglycaemia bursts have adverse effects of numerous organs in the human body, including primarily the vasculature and haematopoietic system, both of which collectively contribute to the state of a high CVD risk in those with diabetes.
PPSC (Post-Prandial Sugar Control) and Its Impact on CVD

Despite the fact that the pathophysiological mechanisms by which individuals develop type 1 or type 2 diabetes are different, both these conditions are characterised by elevated blood sugar levels and eventually share a similar, elevated risk when it comes to cardiovascular mortality.
Regardless of the fact that benefits derived from intensive glucose-lowering treatments were quite obvious in the reduction of microvascular complications in initial trials such as DCCT (Diabetes Control and Complications Trial), ACCORD (Action to Control Cardiovascular Risk in Diabetes), and Action in Diabetes and Vascular disease, Preterax and Diamicron MR Controlled Evaluation (ADVANCE) trials demonstrated no obvious benefits from short-term glucose-lowering treatment.
Although new treatments, when it comes to lowering postprandial blood sugar levels, tend to reduce major adverse cardiovascular events (or MACE), it is already quite evident that most of the therapeutic benefits are achieved independently of their reduction in HbA1c. Hence, the extent to which a reduction of high postprandial blood sugar levels in diabetes reduces CVD remains largely controversial.
Although some researchers have noted a modest reduction in CVD risk by glucose-lowering treatment in extremely large meta-analyses, the effects are quite disappointing, with no reduction of all-cause mortality being successfully identified. The reasons for this are not yet completely comprehended; however, it is thought that benefits of glucose-lowering treatments may be counterweighed to a certain extent by an increase in the occurrences of severe episodes of hypoglycaemia, which is associated with intensive insulin therapy.
In fact, controlling traditional risk factors of CVD, including plasma lipids and blood pressure, are still the most successful strategies to reduce CVD mortality in those with diabetes. That said, statins are quite less effective in individuals with diabetes, even if levels of cholesterol are lowered equally. This suggests that there is yet a large unmet medical requirement for optimised CVD risk-management in those with diabetes. The phenomenon that diabetes is primarily characterised by high blood sugar levels and an increased CVD risk, but glucose-lowering treatment cannot reduce this risk is often called the ‘glucose paradox.”
PPSC and Its Impact on CKD
If you have developed diabetes, you must ask your doctor about chronic kidney disease or CKD.
CKD quite often develops in a gradual and slow manner, exhibiting few symptoms. Most individuals do not realise that they have CKD until it is quite advanced and the need for dialysis (a treatment of filtering the blood) or a kidney transplant arises.
If you have developed diabetes, check the health of your kidneys on a regular basis, which is done with simple urine and blood testing. Regular testing is your best bet in the early detection of CKD, if indeed you do develop it. Early treatment is highly effective and can help in preventing additional health complications.
CKD is quite common in those with diabetes. Around one in three adults with diabetes has CKD. Kidney disease can be caused by both type 1 as well as type 2 diabetes.
The Precise Way Diabetes Leads to Kidney Disease
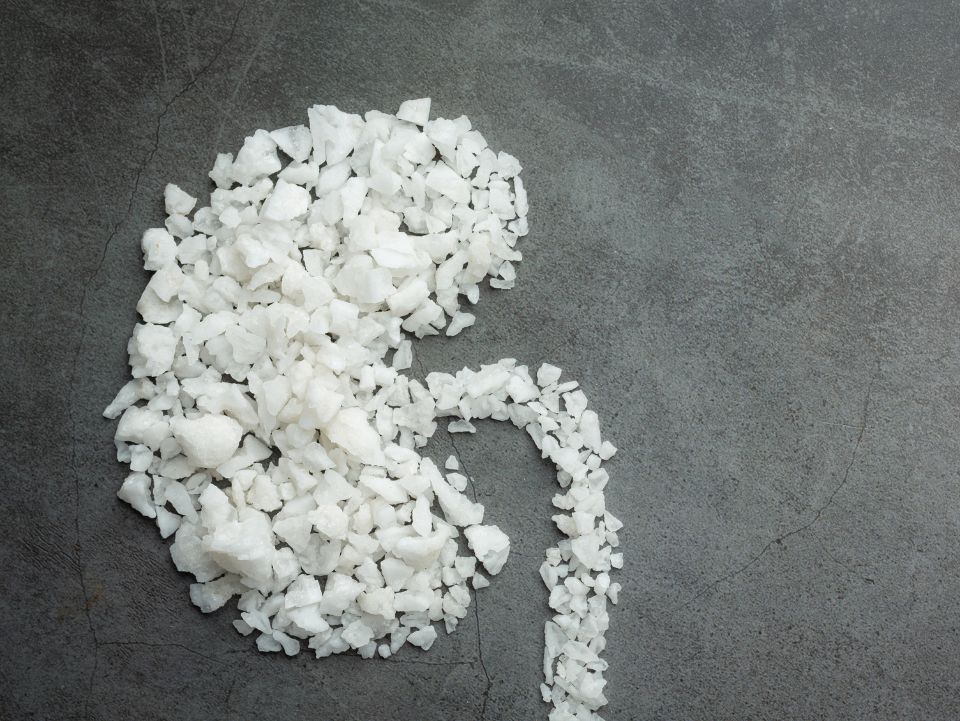
Each kidney in the body is comprised of millions of tiny filters known as nephrons. Over the course of time, high postprandial blood sugar levels (because of diabetes) begin damaging the blood vessels in your nephrons and kidneys, resulting in inefficient functioning of the organ as a whole. Many individuals with diabetes also develop high blood pressure, which can further cause damage to kidneys.
CKD takes a substantially long time to develop, without exhibiting any signs or symptoms during the early stages. You will most probably not know if you have CKD, unless blood and urine tests confirm the condition.
Glucose homeostasis is highly altered in those with CKD, who are exposed to an elevated risk of both hypoglycaemia and hyperglycaemia. Both low and high glycaemic levels are directly associated with shortened survival and increased morbidity in this group of patients.
To Sum It Up:
When postprandial blood sugar normal range is not successfully maintained, it can lead to cardiovascular disease (CVD). That said, there exists something called ‘glucose paradox,” which means that even when a person with diabetes is put on glucose-reducing treatment, it does not reduce the occurrence of CVD. The most efficient glycaemic monitoring as well as control that is tailored for those with diabetes is required to prevent hypoglycaemia and several other glycaemic disarrays in those with diabetes and CKD. Understanding renal physiology and the pathophysiology of CKD has become essential to all specialties that treat diabetic individuals.
References:



